You can put some more descriptive text about the page or an introduction to its content to get the reader excited right here.
This section features a list of features or benefits on the left and an image on the right. I recommend using a portrait or square image for the best performance at various device sizes. You’ll want to use a PNG file with a transparent background.
BCI handles all the heavy lifting of your benefits and HR needs. From enrollment communications to data exchange and expert advising, we have you covered so you can focus on the future of your business.
Satisfied employees are crucial to your company. That’s why we’ve developed an employee assistance program that assists them with their HR needs and offers everything from one-on-one meetings.
We work at lightning speed. With BCI, implementation is 4 times faster than if you were implementing benefits on your own. Faster implementation saves you time and money!
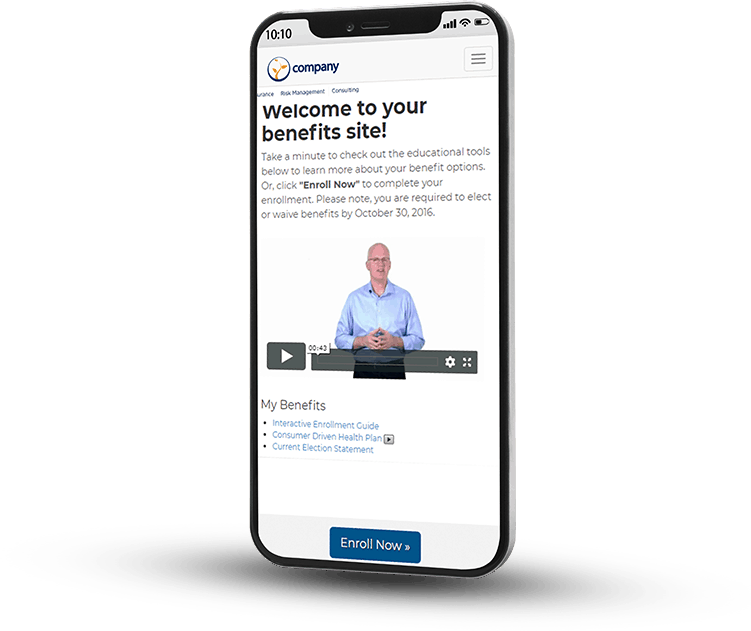
Whether you have an annual or newly eligible enrollment, we are here to walk you and your employees through the enrollment process, answer any questions, and facilitate implementation.
This is a simple text section with a headline. It is more narrow than other sections that feature multiple columns and module types.
Paria sunt igitur. Ut aliquid scire se gaudeant? Oratio me istius philosophi non offendit; Conferam tecum, quam cuique verso rem subicias; Itaque ad tempus ad Pisonem omnes.
Comprehensum, quod cognitum non habet? Maximas vero virtutes iacere omnis necesse est voluptate dominante. Praeteritis, inquit, gaudeo. In eo enim positum est id, quod dicimus esse expetendum. Et quod est munus, quod opus sapientiae? Conferam avum tuum Drusum cum C.
This section features a list of features or benefits on the left and an image on the right. I recommend using a portrait or square image for the best performance at various device sizes. You’ll want to use a PNG file with a transparent background.

BCI handles all the heavy lifting of your benefits and HR needs. From enrollment communications to data exchange and expert advising, we have you covered so you can focus on the future of your business.
Satisfied employees are crucial to your company. That’s why we’ve developed an employee assistance program that assists them with their HR needs and offers everything from one-on-one meetings.
We work at lightning speed. With BCI, implementation is 4 times faster than if you were implementing benefits on your own. Faster implementation saves you time and money!
Whether you have an annual or newly eligible enrollment, we are here to walk you and your employees through the enrollment process, answer any questions, and facilitate implementation.

Counselor assistance both onsite and call center-based with dedicated full-time Benefit Representatives.

Manage newly eligible employees through our new hire enrollment plans to meet your specific needs.

Self-service through BCI’s wholly-owned enrollment system with BCI educational modules, decisions tools and voluntary benefit enrollment integration.
Discover how we can help empower your employees and your company toward a brighter future!